
Claims Processing Capability
RenumerMed provides extensive claims processing capability including:
- Process to clearinghouses, insurance carriers, Medicaid, Medicare, and Blue Cross / Blue Shield, etc.
- Ability to submit and track the status of primary, secondary and tertiary claims
- View and edit claims prior to submission
- Built-in claim checker detects potentially faulty claims prior to submission
- Claim files display patient co-pay amounts
- Establish claim defaults on a patient-by-patient basis
- Manage claim authorizations and insurance eligibility
Payment Options
Payments can be logged and received in a number of ways including:
- Bill HCFA 1500 and UB92 claims
- Multiple forms of payment posting into proper patient’s file, including automatic posting and manual entry
- Post and track capitation payments by insurance carriers
- Post single or batch payments
- Track patient charges and remittance history
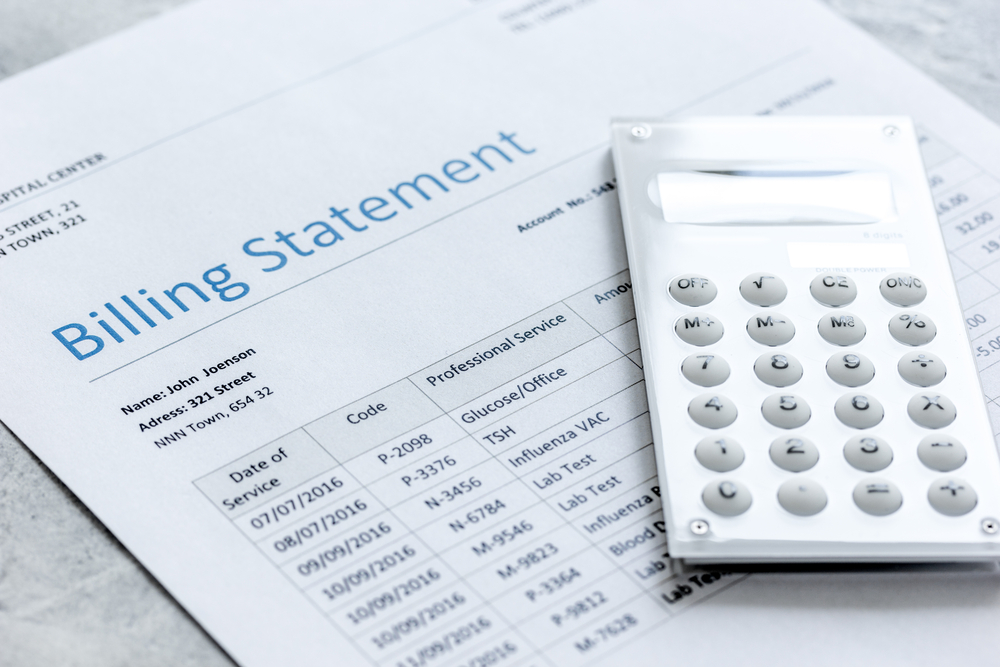
Automatic Billing Statements
Billing statements are issued automatically and provide for:
- Generation of receivables summary and viewing of unpaid claims by doctor, patient, date, etc.
- Generation of patient invoices and statements, individual or batch
- Creation of EDI claim remittance notices based on carrier
Billing Process Customization
In addition to the pre-set functions above, RenumerMed provides for customization of billing processes through:
- EDI modules for connectivity to a variety of payers and clearinghouses
- Set parameters for moving unpaid visits into collections
- The ability to create and edit an unlimited number of fee schedules
- A unique interest charging window that provides the ability to post interest charges to existing claims
- Establishment of criteria for recurring claim processing
- Establishment of uniform charges for commonly used procedure codes
- A special interface that provides connectivity to external accounting software packages, from Quickbooks and Peachtree to Oracle and SAP
- Patient’s co-pay amount conveniently displayed in patient record

